If you’ve been following along with my blog, you know I’m an Occupational therapist that works with kids with neurodiversity. In 2020 I started mentoring in my role as a preceptor for Occupational therapy and Occupational therapy assistant students in their programs. I remembered how big and scary the world can be graduating from school and trying to figure out what to do and where to go with your education. I realized that one thing I can do is try to use my blog to make things a little easier.
I have reached out to some friends and colleagues to help share their roles and scope of practices in the occupational therapy profession, and I will be writing different articles about the different populations and roles you might see an occupational therapist working in. My hope is that people will be able to read, learn and share about occupational therapy so that more people will be able to seek out services if it would benefit them.
This post is going to be about one of my friend’s roles, she is an Occupational therapist in a Regional treatment centre. Individuals that access these centres are inmates with serious mental health conditions and access in patient therapies. She works on an interprofessional team of psychiatrists, physicians, psychologists, social workers, behavioural science technicians, nurse practitioners, nurses, PSW’s, pharmacists and of course, Occupational therapists. I’ve put together this blog with the questions I asked my friend and her direct answers to them – if you have other questions you’d like to know add them in the comments!
Also, Occupational therapy is very jargon heavy, so I left the answers my friend wrote as is, and added a mini glossary to the bottom of this post to help out!
What kind of goals do you work with your clients towards ?
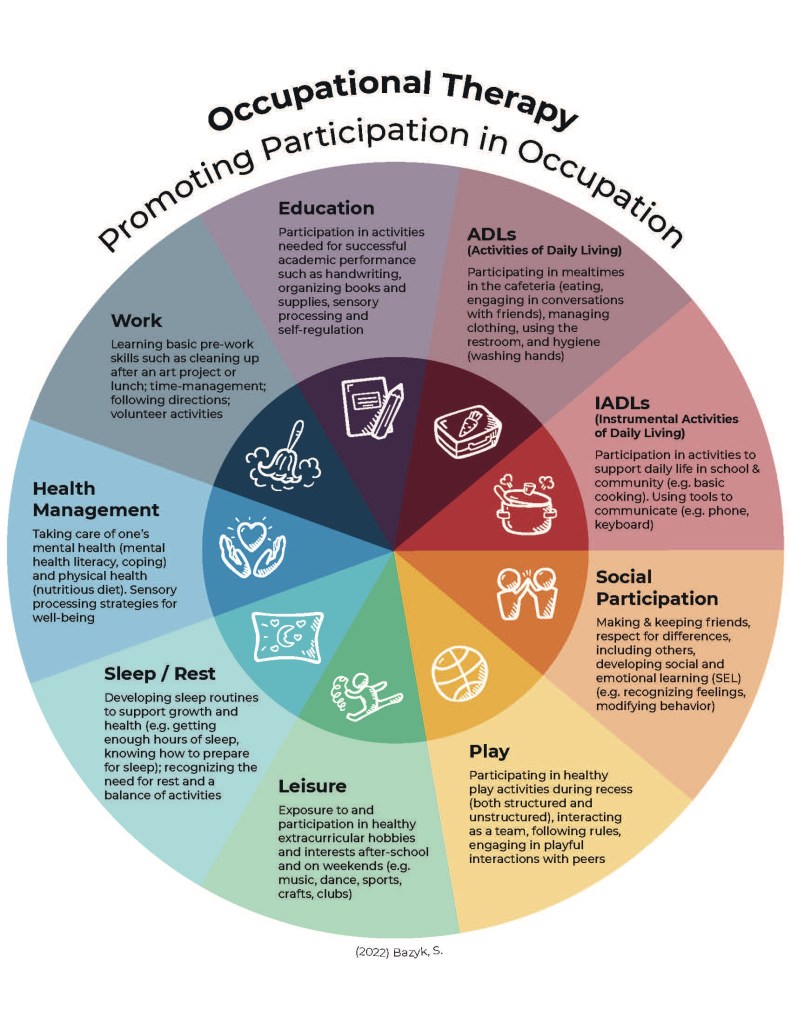
- Occupational Therapists work under the Mental Health Department of Health Services. Our role is unique in that we work very closely with the clinical health services team as well. We have individual clients where we are the “clinical case coordinators” which involves individual therapy, as well as a case management type role. (My addition in case anyone is curious – Case managers facilitate patient care by assessing patient needs, evaluating treatment options, creating treatment plans, coordinating care and assessing progress). We also get specific OT scope referrals. These involve assessment, and then a determination if recommendations can be carried out by other professionals or involve time-limited OT intervention for specific goals. The goals are set collaboratively with our clients. If our clients have acute mental health needs, we focus on mental health symptom stability, distress tolerance and coping. We also address suicide, self injury, addiction and other mental health symptoms. Some other areas we address from a more top of scope OT perspective include: ADL’s (activities of daily living), IADL’s (Instrumental activities of daily living), sensory processing, mobility and seating, cognitive screening.
Do you use any specific theories/techniques/strategies in your role
- We have taken additional trainings to be able to incorporate psychotherapeutic modalities (e.g. ACT, CBT, DBT, MI). We take ongoing training on suicide and self injury. A main model used is The interpersonal-psychological theory of suicidal behavior (Joiner, 2005). I try to focus on rapport building initially before diving into specific therapies.
- Also, its important to have personal mental health management strategies (coping strategies for YOU as a therapist) as the role can be stressful and sometimes involve exposure to traumatic situations, themes etc.
Do you have a recommended book/course/learning themes that people can look into in order to learn more for that role
- I recently took and enjoyed the CAOT Dementia Care Dealing with Responsive Behaviours Workshop and OSOT Cognitive Stimulation Therapy Workshop. Psychwire does have some easy to follow self-directed learning and provides manuals and resources. I enjoyed the Intro to Acceptance and Commitment Therapy course. University of Alberta also has a 6 week Seating and Mobility Assessment course which might be helpful for new therapists or those wanting a refresher on this area if they have not worked in physical health for a while.
Anything else you think a new grad looking into what area of OT they’d want to go into would like to know
- Don’t be afraid to reach out to OTs and ask questions! If you are an Ontario resident, you can go to the COTO website and all of the OTs are listed there by their population and practice. COTO is our regulating body, so if you are living outside of Ontario, the regulating body of that region should have something similar! You can also find OTs on LinkedIn, Instagram, Twitter etc. Many of us are lovely to talk to and eager to answer questions!
Glossary:
ADLs – Activities of daily living – eating, bathing, toileting etc
IADLs – Instrumental activities of daily living – cooking, house cleaning etc
ACT – Acceptance and Commitment Therapy
CBT – Cognitive Behavioural Therapy
DBT – Dialectical Behavioural Therapy
MI – Motivational Interviewing
If you have any questions further about occupational therapy or if you have experiences you would like to share, please feel free to reach out by leaving a comment below! I will try to continue working on these posts, so if you think I am missing anything or would like to share your personal experience working at a Regional Treatment Centre, send me a blurb to add!
More of my OT related blogs to check out!
The Role of Occupational Therapists: The ACT Team
October is Occupational Therapy Month!